Navigating Prosopagnosia Treatment: Hope Beyond Face Blindness
Imagine a world where every face you encounter feels new, unfamiliar, and indistinguishable from the last. This isn't a scene from a science fiction movie, but the daily reality for individuals living with prosopagnosia, often referred to as "face blindness." This neurological condition profoundly impacts one's ability to recognize familiar faces, including those of family, friends, and even one's own reflection. The challenges it presents are immense, affecting social interactions, personal safety, and overall quality of life. Understanding the nuances of prosopagnosia treatment is crucial for those affected and their loved ones, offering pathways to better manage this complex disorder.
While the concept of face blindness might seem abstract to many, its real-world implications are deeply personal and often isolating. From navigating crowded public spaces to simply recognizing a loved one across a room, daily tasks become monumental hurdles. This article aims to demystify prosopagnosia, exploring its causes, symptoms, and, most importantly, the current approaches to prosopagnosia treatment. We will delve into the strategies and insights that empower individuals to adapt and thrive, even in the absence of a definitive cure.
Table of Contents
- Understanding Prosopagnosia: More Than Just Forgetting a Face
- The Core Challenge: Is There a Cure for Prosopagnosia?
- Spontaneous Recovery in Acquired Prosopagnosia: A Glimmer of Hope?
- The Foundation of Prosopagnosia Treatment: Compensatory Strategies
- Living with Prosopagnosia: Practical Coping Mechanisms
- The Role of Diagnosis in Effective Management
- Research and Awareness: Paving the Way Forward
- Expert Insights and Resources for Prosopagnosia Treatment
Understanding Prosopagnosia: More Than Just Forgetting a Face
Prosopagnosia, derived from the Greek words "prosopon" (face) and "agnosia" (lack of knowledge), is precisely what its name implies: the inability to recognize faces. It's a selective visual agnosia, meaning the difficulty is specific to faces, while other visual recognition abilities might remain intact. This neurological condition typically arises due to problems or damage in specific brain regions, particularly the inferior occipital region, fusiform gyrus, and temporal cortex, which are crucial for facial processing. It's not about memory loss or impaired vision; it's a profound deficit in the brain's ability to process and identify facial identity.
- Leave It Beaver Cast
- Recent Pictures Of Marlo Thomas
- Whoopi Goldberg Net Worth
- Rocky Cast
- What Happened To Kathleen Turner Health
There are two primary forms of prosopagnosia: acquired and developmental. Acquired prosopagnosia results from brain damage, often due to stroke, head injury, neurodegenerative diseases, or other neurological conditions. In contrast, developmental prosopagnosia (also known as congenital prosopagnosia) is present since birth, with no known brain injury. Individuals with developmental prosopagnosia report severe, lifelong difficulties recognizing facial identity. Understanding these two forms and their symptoms is the first step toward seeking proper diagnosis and exploring potential prosopagnosia treatment strategies.
The Core Challenge: Is There a Cure for Prosopagnosia?
One of the most pressing questions for anyone affected by face blindness is whether a cure exists. The direct answer, unfortunately, is that there is currently no known cure for prosopagnosia. So far, there isn’t one specific form of treatment for prosopagnosia that can completely reverse the condition. This holds true for both developmental prosopagnosia, which is usually permanent, and acquired forms, where full recoveries aren't common.
The medical community widely acknowledges that there are no cures for prosopagnosia in the traditional sense. This reality can be disheartening for individuals and families navigating the challenges of face blindness. However, it's crucial to understand that "no cure" does not mean "no hope" or "no help." The good news is that while a cure remains elusive, treatment can significantly help a person with this condition. The focus shifts from curing the underlying neurological deficit to empowering individuals with effective strategies to manage their daily lives and improve their ability to identify others. This distinction is vital for setting realistic expectations and pursuing beneficial interventions.
- Mary Anne Owen
- Height Of Jason Alexander
- Dolly Parton Bathing Suit
- Marie Osmond Net Worth
- Jennifer Angel Horoscopes
Spontaneous Recovery in Acquired Prosopagnosia: A Glimmer of Hope?
While the general outlook for a complete cure for prosopagnosia is dim, particularly for congenital cases, there is a nuanced aspect concerning acquired prosopagnosia. It is important to note that some of the causes of acquired prosopagnosia are curable. For instance, if face blindness results from a treatable brain tumor, an infection, or a reversible metabolic disorder, resolving those underlying problems might help with this condition. In such rare instances, addressing the root cause can sometimes lead to an improvement or even a resolution of the facial recognition difficulties.
However, it is equally important to manage expectations. Even when the underlying cause of acquired prosopagnosia is treatable, these recoveries aren't common, and the degree of improvement can vary significantly. The current literature on spontaneous recovery in acquired prosopagnosia (AP) suggests that while it can occur, it is not the norm. Most individuals who develop prosopagnosia due to brain damage will experience persistent difficulties. Therefore, while there's a glimmer of hope for some acquired cases, the primary approach to prosopagnosia treatment still largely revolves around adaptive and compensatory strategies rather than curative interventions.
The Foundation of Prosopagnosia Treatment: Compensatory Strategies
Given that there is no known cure for prosopagnosia, the cornerstone of prosopagnosia treatment lies in developing robust compensatory skills. Treatment focuses on "workarounds" and other coping skills that can assist prosopagnosics in identifying other people. The goal is not to "fix" the brain's ability to recognize faces, but rather to equip individuals with alternative methods for recognizing individuals, thereby minimizing the daily impact of face blindness. This approach is mainly supportive and involves developing coping mechanisms to help manage the condition better.
The focus of any treatment should be to help the individual with prosopagnosia develop compensatory strategies. These strategies empower individuals to learn other ways of remembering faces and distinguishing people, moving beyond reliance on facial features alone. The good news is that with dedicated effort and appropriate guidance, people with prosopagnosia can significantly improve their ability to navigate social and professional environments. The current treatment options for prosopagnosia primarily include cognitive rehabilitation therapy, compensatory techniques, and face processing training, all aimed at bolstering these alternative identification methods.
Beyond Faces: Utilizing Other Cues
Since facial recognition is impaired, individuals with prosopagnosia must learn to rely on other identifying features. This involves consciously shifting attention away from faces and towards a holistic perception of a person. Key compensatory techniques include focusing on:
- Voice: Recognizing a person by the sound, pitch, and unique inflections of their voice.
- Hair: Distinctive hairstyles, color, or length can be powerful identifiers.
- Gait and Body Language: The way someone walks, their posture, and their characteristic gestures can be unique cues.
- Clothing and Accessories: While temporary, a person's typical style, specific outfits, or accessories like glasses or jewelry can aid recognition in familiar contexts.
- Context and Location: Remembering where you usually encounter someone (e.g., "the person I see at the coffee shop," "my colleague from the marketing department") can provide vital clues.
- Unique Physical Features: Scars, birthmarks, tattoos, or a distinctive nose shape (though not part of overall facial recognition) can be used as specific, non-holistic identifiers.
Cognitive Rehabilitation Therapy and Face Processing Training
Cognitive rehabilitation therapy plays a significant role in prosopagnosia treatment. This therapy aims to strengthen other cognitive functions that can indirectly aid in person recognition. For instance, memory training might help individuals better recall non-facial details associated with a person. Problem-solving skills can be honed to develop systematic approaches to identification in challenging situations. These therapies are tailored to the individual's specific needs and the type of prosopagnosia they experience.
Furthermore, face processing training, while not a cure, is an area of ongoing research and intervention. These programs are aimed at exploring potential interventions to improve specific aspects of facial processing, even if holistic recognition remains difficult. For example, training might involve focusing on individual facial features (like eyes or mouth) in isolation, or practicing matching faces to names repeatedly. While these trainings haven't shown to "cure" prosopagnosia, they can sometimes lead to marginal improvements in specific tasks or help individuals develop more efficient compensatory strategies. Experts continue to explore and refine these cognitive training programs, hoping to unlock new avenues for support.
Living with Prosopagnosia: Practical Coping Mechanisms
Beyond formal therapies, successful prosopagnosia treatment heavily relies on developing practical, everyday coping mechanisms. Treatment of prosopagnosia is mainly supportive and involves developing coping mechanisms to help manage the condition better in real-world scenarios. Those with prosopagnosia must learn other ways of remembering faces, and this often involves a combination of personal strategies, environmental adaptations, and effective communication with others.
For many, living with face blindness means constantly being on alert for non-facial cues. It can be exhausting and lead to social anxiety or avoidance. Therefore, fostering resilience and self-advocacy is a crucial part of managing the condition. This involves not only learning identification strategies but also developing the confidence to explain the condition to others and ask for help when needed. The treatments are given to focus on the coping mechanism that may be helpful in identifying individuals better, making daily life more manageable and less stressful.
Social Strategies and Communication
Navigating social situations can be particularly challenging for individuals with prosopagnosia. A key coping mechanism is open communication. Explaining the condition to friends, family, and even new acquaintances can alleviate awkwardness and foster understanding. Simple phrases like, "I have trouble recognizing faces, so please say your name when you greet me," can make a significant difference. Other social strategies include:
- Asking Direct Questions: If unsure, it's often better to politely ask, "Have we met before?" or "Could you remind me of your name?"
- Using Context Clues: In group settings, listening to conversations and observing interactions can provide context to identify speakers.
- Pre-planning: Before social events, asking a trusted companion to point out key individuals can be helpful.
- Creating Mental Files: Associating people with specific details (e.g., "Sarah from accounting, always wears bright scarves") can aid recall.
Technological Aids and Future Directions
While there is currently no specific treatment for prosopagnosia, ongoing research is being conducted to explore potential interventions, including the role of technology. Although not a "cure," technological aids can offer practical support for individuals with face blindness. For example, some individuals use their phone cameras to take pictures of people they need to remember, adding notes about their name and identifying features. Facial recognition apps, while primarily designed for security or convenience, could potentially be adapted for personal use by individuals with prosopagnosia, though privacy concerns and ethical considerations would need to be addressed.
The field of neuroscience and cognitive science is continually advancing. Researchers are exploring various avenues, such as brain stimulation techniques (e.g., transcranial magnetic stimulation or TMS) and virtual reality environments for targeted training programs. While these are still largely experimental, they represent the future frontier of prosopagnosia treatment research, offering hope for more direct interventions or significantly enhanced compensatory tools in the years to come. The aim is to leverage new discoveries to better understand and, eventually, mitigate the challenges of face blindness.
The Role of Diagnosis in Effective Management
Before any prosopagnosia treatment can be considered, accurate identification and diagnosis are paramount. Understanding the symptoms and how to receive a diagnosis can be a way to find proper treatment strategies. Prosopagnosia can arise from brain damage or be present since birth, and distinguishing between acquired and developmental forms is crucial for appropriate management.
Diagnosis typically involves a series of specialized tests administered by neurologists, neuropsychologists, or cognitive scientists. These assessments evaluate a person's ability to recognize faces, often comparing it to their ability to recognize other objects. One of the most common diagnostic assessments is the Cambridge Face Memory Test (CFMT), which measures an individual's ability to learn and recognize novel faces. While developmental prosopagnosia is characterized by severe, lifelong difficulties, a comprehensive diagnosis helps confirm the condition and rule out other underlying issues. To begin addressing such issues, experts suggest starting with practical ways to identify prosopagnosia, moving towards better awareness, and then focusing on treatment of the condition. A formal diagnosis provides clarity, validates the individual's experiences, and opens the door to appropriate support and compensatory training.
Research and Awareness: Paving the Way Forward
The journey of prosopagnosia treatment is deeply intertwined with ongoing research and increasing public awareness. Organizations like the Prosopagnosia Research Center at Dartmouth, Harvard, and the University of London, along with platforms like Faceblind.org, aim to provide a better understanding of prosopagnosia to the public. Their efforts are crucial in disseminating information, supporting research, and connecting individuals with resources.
Through dedicated research, scientists are continually gaining deeper insights into the neurological underpinnings of prosopagnosia. Advances in brain imaging and cognitive neuroscience are helping to localize the specific brain regions involved, such as the inferior occipital region, fusiform gyrus, and temporal cortex. This enhanced understanding is vital for developing more targeted and effective interventions. Furthermore, raising awareness of this disease, as experts from PSRI have tried to do by providing detailed insight into prosopagnosia types and symptoms, helps reduce stigma, encourages early diagnosis, and ensures that individuals receive the support they need. The more the public understands face blindness, the more inclusive and accommodating society can become for those living with it.
Expert Insights and Resources for Prosopagnosia Treatment
The field of prosopagnosia treatment is continuously evolving, driven by the dedication of researchers and clinicians worldwide. Experts like Punit Shah, affiliated with MRC Social, Genetic, and Developmental Psychiatry Centre, King's College London, have contributed significantly to the literature on the identification, diagnosis, and treatment of prosopagnosia. Their work, alongside numerous other specialists, underpins the current understanding and management strategies for this complex neurological disorder.
For individuals seeking more information or support, a wealth of resources exists. Reputable academic institutions and research centers often provide detailed insights and connect individuals with ongoing studies or clinical trials. Websites dedicated to prosopagnosia, often maintained by research groups, offer valuable information on causes, symptoms, diagnosis, and the latest treatment options. Engaging with these expert-driven resources is crucial for anyone looking to learn about the current literature on spontaneous recovery in acquired prosopagnosia (AP), as well as treatment attempts in acquired and developmental prosopagnosia (DP). While a definitive cure remains elusive, the collective knowledge and ongoing efforts of the scientific community provide a strong foundation for managing prosopagnosia and improving the lives of those affected.
Conclusion
Prosopagnosia, or face blindness, is a profound neurological condition that presents unique challenges in recognizing faces. While the current medical consensus is that there is no known cure for prosopagnosia, particularly for its developmental form, hope and effective management are certainly within reach. The core of prosopagnosia treatment revolves around developing robust compensatory strategies, enabling individuals to identify people through non-facial cues like voice, gait, and context. Cognitive rehabilitation therapy and ongoing research into face processing training also play vital roles in supporting those affected.
Living with prosopagnosia requires adaptability, resilience, and often, open communication with others. By understanding the condition, seeking accurate diagnosis, and actively implementing coping mechanisms, individuals can significantly improve their quality of life and navigate social interactions more confidently. The continuous efforts in research and public awareness are paving the way for better understanding, more refined interventions, and a more inclusive society for those with face blindness. If you or someone you know is struggling with prosopagnosia, we encourage you to explore the resources mentioned and consult with neurological specialists. Share this article to help raise awareness and support those living with this often-misunderstood condition.

Understanding Prosopagnosia - Faceblind
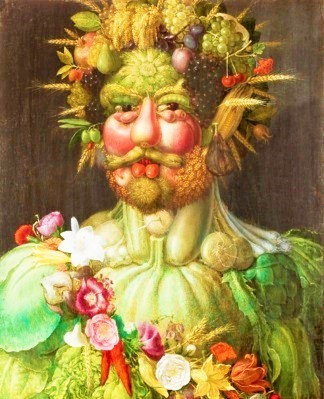
野菜王子であり、果物王子だったルドルフ2世の驚異の世界こそ脅威! | ファンファン福岡

immaginare